35 year old male patient came to causality with the c/o vomitings 3days back (10episodes), associated with blood
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome
35 year old male patient came to causality with the c/o vomitings 3days back (10episodes), associated with blood
HOPl:-
patient was apparently asymptomatic 3days back then he developed vomiting (10episodes) associated with blood,h/o alcohol consumption 3dyas back
no history of bleeding per rectum, abdomen distension, pedal edema,no other complaints.
Past History:
Not k/c/o DM,HTN,TB,Asthma,CVA,CAD,Epilepsy
Personal history:
Occasional alcoholic since 10years
O/E:
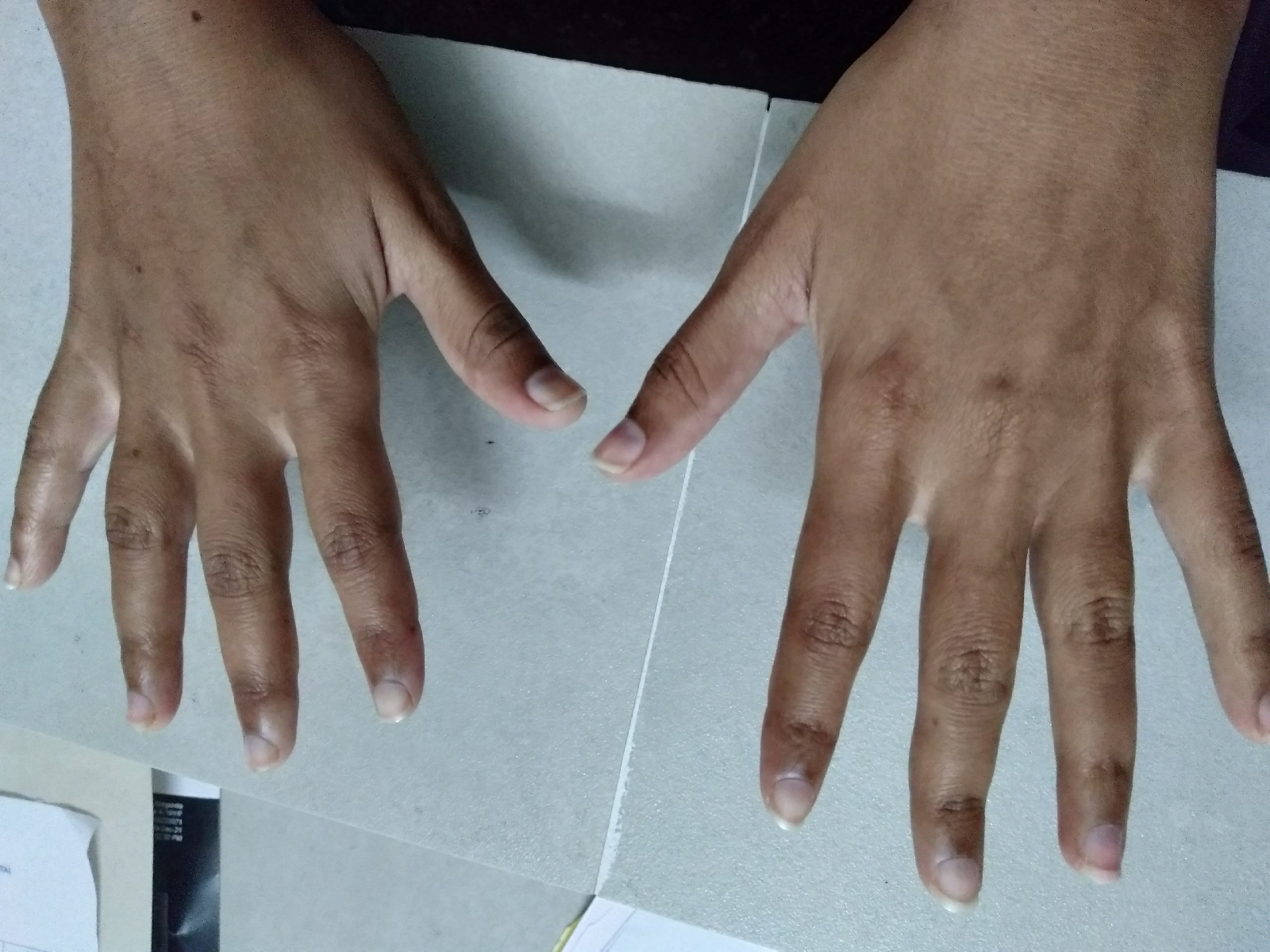
No pallor/Icterus/cyanosis/clubbing/Generalized lymphadenopathy/pedal edema
Temp-afebrile
PR- 100bpm
RR-24/min
BP-130/110 mmhg
Spo2- 98%at RA
GRBS-140 mg/dl
CVS- S1 S2 +,No murmurs
RS- BAE+,nvbs +
P/A- soft, non tender
CNS- NAD
Investigations:-
GI Endoscopy
Chest X ray
2D ECHO
USG
ECG
Provisional diagnosis:-
OESOPHAGEAL ULCER 2° TO REFLUX OESOPHAGITIS (GRADE || ) ALCOHOL INDUCED
TREATMENT;-
1)NBM TILL FURTHER ORDER
2)IVF 0.9&DNS WITH 1AMPOULE OPTINURON/IV/OD
3)INJ.PAN 200mg IV IN 50CC@2CC/HR (8mg/hr)
4)TAB.RANITIDINE 150mg /BD
5)INJ.VITAMINE K 1AMPOULE /IV/OD
6)INJ.TRANEXA 500mg /IV/BD
7)T.LEVOSULPRIDE 25 mg/BD
8)T.HP KIT/BD (OMEPRAZOLE +AMOXICILLIN +TINIDAZOLE)
9)SYP.MUCAINE GEL 10ml /PO/TID